“Healthcare systems and individual practices will need to be redesigned to support routine UDT” (Bair and Krebs 2010)
 HARMS Program
HARMS Program
The HARMS Program is a clinic-wide system built to support routine urine drug testing (UDT) as a method of monitoring safety in patients prescribed opioids for chronic non-cancer pain. First implemented in clinical practice in 2014-15, it has went on to receive numerous awards at the provincial and national levels for innovation and scalability. HARMS is based on the principle that UDT results can be seen as indicators of risk, and may adjust the risk/benefit balance of these medications and change if and how these are prescribed and further monitored. UDT may help identify risks sooner, including addiction to opioids, and adjust management to meet the needs of the patient. UDT is certainly not the only marker of risk, and must be used as part of a clinical Gestalt to guide patient discussion, however it is an important enough component that it is recommended by numerous national and international guidelines. Unfortunately, UDT is not commonly done in practice due to numerous logistical barriers. HARMS was built in a resource-limited setting to address these barriers in an efficient way. This includes improving efficiency, adherence to best practices, and accuracy of interpretation through the core program features of: automation (START-IT Tool), delegation to non-medical staff members (protocols), and simple and versatile clinical algorithms to guide action (HARMS Risk Ladder). It has been refined and studied and early results suggest it is effective at identifying patients who are at risk, and changing management (including starting treatment for addiction). Clinical expansion has begun, and further research including a pending feasibility study for further expansion and evaluation.
 START-IT
START-IT
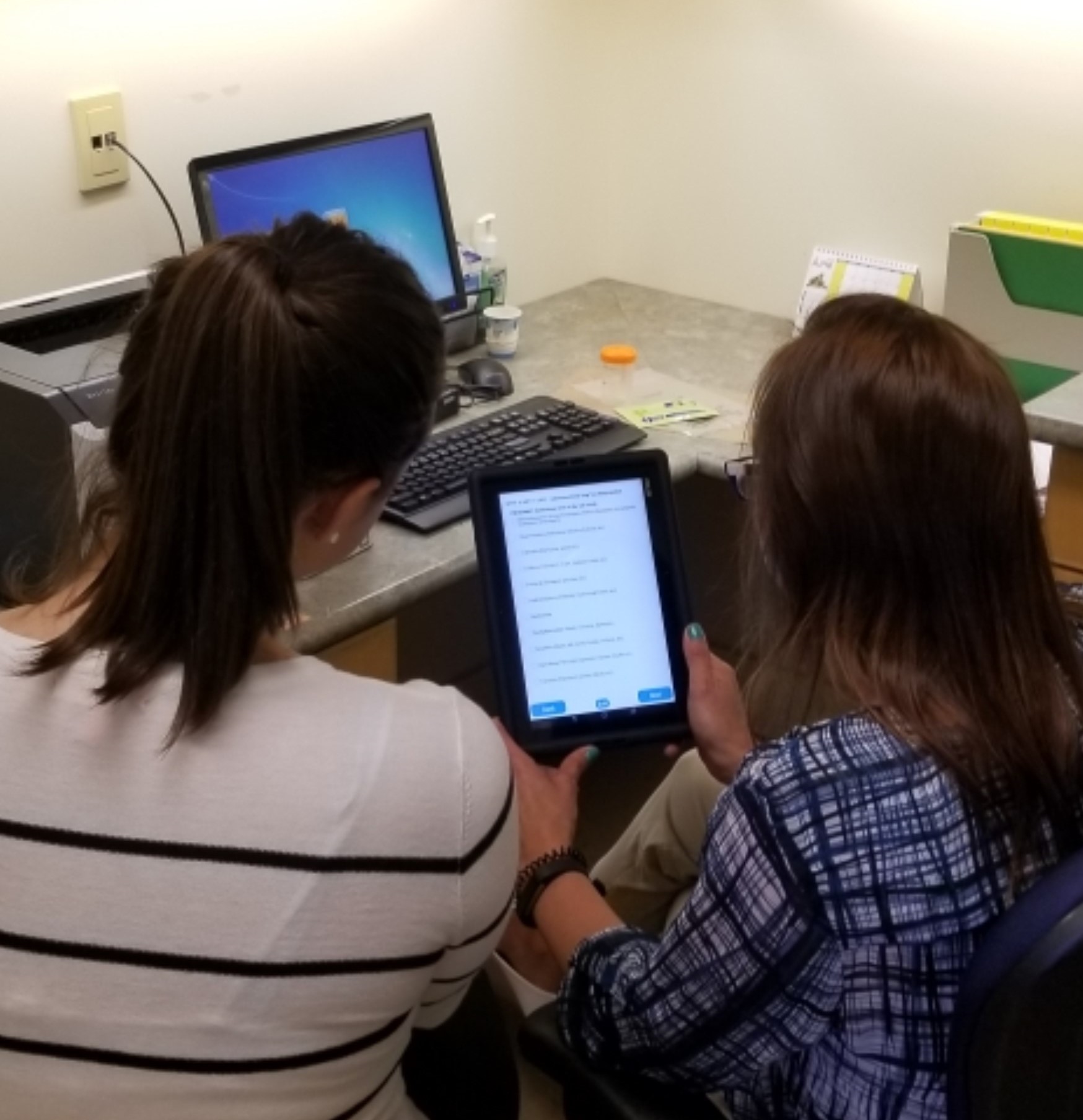
START-IT (Self-report, Testing, and Automated Reading Tool for Immunoassay Tests) was designed to simplify the process of UDT in the office. It uses a tablet PC to collect the required information for a UDT, and then interprets that information within the limitations of the test. START-IT provides a customized, pragmatic report indicating exactly what this result may mean for this specific patient, as well as additional considerations for the clinician given the inherent limitations of UDT. The report is synchronized with the electronic medical record (EMR) with the click of a button. START-IT also tracks data which can be used for quality improvement and research purposes. The automation of START-IT ensures that no medical personnel are required for the administration of urine drug testing, IA interpretation, or even in making the decision to send for confirmatory testing with LC-MS. This is an important part of the HARMS Program in that it makes UDT less burdensome for physicians and therefore more practical in frontline medicine.
 UrInterpret
UrInterpret
UrInterpret is an app we made for smartphones that is intended to be a quick aid when interpreting UDT (immunoassay and/or liquid chromatography-mass spectrometry). Within a few clicks, you can find out answers to questions such as: my patient is prescribed morphine, what IA panels should show up positive? Or, my patient unexpectedly had the benzodiazepine panel show up positive, what might have caused this? Or, my patient is prescribed morphine, what metabolites might I see on LC-MS that are from this medication versus metabolites that should not be seen with morphine and imply that my patient took something else? Or, my patient's LC-MS was positive for hydromorphone, what medications may cause this metabolite to show up in the urine? Or, LC-MS results came back positive for methcathinone which a quick google search tells me is a recreational street drug - should I be concerned or is there another explanation for what may have caused this?
