Now that patients are booked for UDT, we will cover considerations for conducting UDT in the office…
Most primary care clinics are not set up to collect UDT (protocols for providing the sample, anti-tampering measures, testing kits, storage of samples, sending to the lab for confirmatory testing, etc.). This section assumes that the UDT is being conducted, and analyzed with IA, on the clinic premises. Note that depending on clinic preferences and patient circumstances, you may consider allowing patients to provide the sample directly at the lab.
Clinic Setup
As discussed further in Appendix I, consider holding “UDT Clinics” a few half-days per week, in which patients are booked sequentially in blocks. This will minimize the effort of setting up the washroom repeatedly as would be required if UDT appointments were booked sporadically throughout the week. We book patients every 20 minutes but in our experience the appointment typically takes less than 10 minutes. Ideally there is a washroom within the clinic that can be used solely for UDT for the duration of the UDT Clinic; this washroom should be close to an exam room. To prepare the facilities for a UDT clinic, we place an “out of order” sign on the door so that its use is reserved during that time for the UDT appointments. Your clinic may also consider anti-tampering strategies which are discussed in Appendix III (blue water, taping faucets, etc.).
START-IT Tool for Simplified UDT
We would strongly encourage you to consider using START-IT to facilitate UDT in your office. We developed this tool, have used it in our own clinic for years, refined it, and share it freely with others. Described further in Chapter 7, START-IT is a program on a tablet PC that simplifies nearly every aspect of UDT in the primary care clinic. Among others, START-IT collects information important for the interpretation of the UDT including prescribed opioid and last dose, non-prescribed drugs/medications, and results of the IA UDT. Prior to this, we collected patient self-reports on paper which created numerous extra steps for physicians and administrative staff alike. A future version of START-IT is also planned to have the capability to automate numerous other components of UDT and Chronic Pain management such as risk stratification, UDT consent, Brief Pain Inventory, and more.
Patient Arrival
For discreteness, appointments are conducted very similar to any other appointment. When patients arrive, they first register for the appointment and wait until they are called into an exam room. We welcome the patient and explain the nature of the appointment if it’s the patient’s first time, and then start using the START-IT tool. If consent is going to be collected with every UDT visit, then the future START-IT tool will be able to facilitate this. Historically we have not been collecting consent at each visit as we obtain a single consent when starting the program, however we would recommend considering it in the future (Appendix IX).
We start by completing the initial parts of START-IT on the tablet PC – prescribed medication and self-reported drugs/medications not prescribed. When applying START-IT, it is important for the clinic employee to verify the prescribed medication (either by entering it personally or double-checking in the EMR what the patients enters).
This is a necessity as the START-IT interpretation will assume this information is accurate. For example, if a patient that is not prescribed oxycodone claims on START-IT that he/she is, then when oxycodone shows up in his/her urine it will appear to be expected.
The patient will then be asked to provide a urine sample.
Provision of UDT
The patient is given a urine-specific container and escorted to the washroom. We use the same containers that are used for urine C&S samples. He/she is asked to provide enough fluid to fill the specimen container to the black line, which is 30mL. In our experience however the lab has been able to process less than 30mL. The patient then brings the sample back to the exam room where it will be analyzed.
 Analysis of UDT
Analysis of UDT
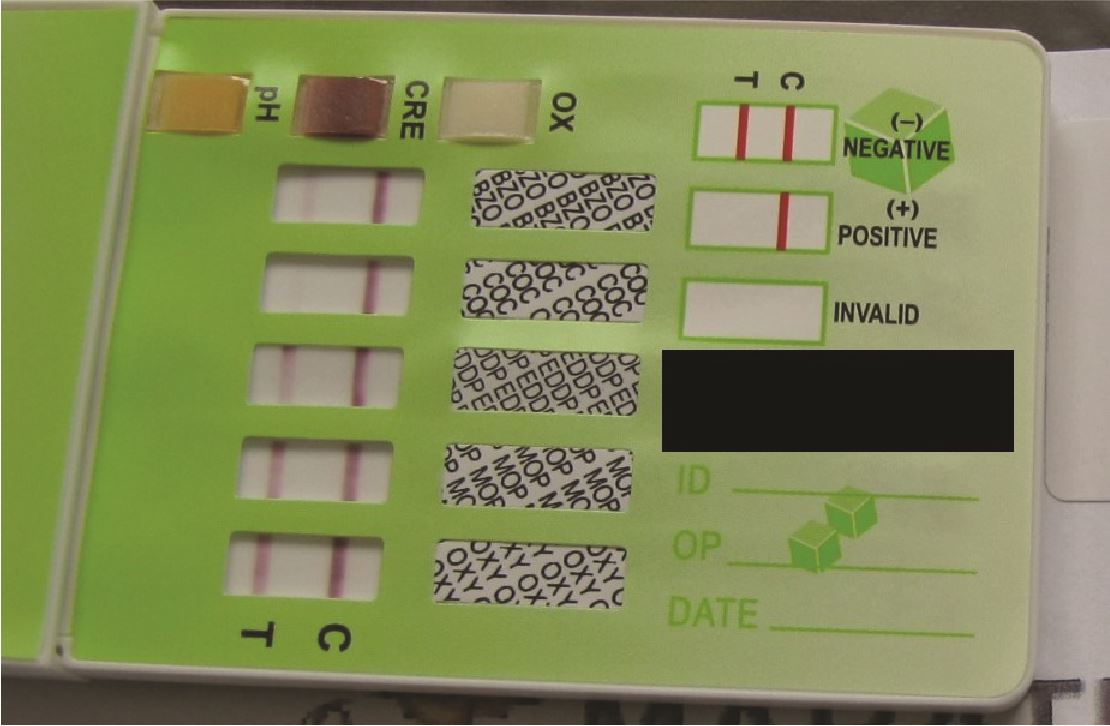
The sample is analyzed with the IA panel(s). Insert the panels into the specimen container (we have to squeeze the container to bend it so that the whole UDT panel kit will fit inside). Leave the panels in for 10-15 seconds. Most panels will have “positive” (a single line), “negative” (a double line) or “invalid” (no lines). Note that even if the 2nd line is very faint, this is still a 2nd line and is considered negative.
If using anti-tampering measures, the temperature should be checked within the first 4-5 minutes of provision and should be 32.2-37.7C. Also urine can be dipped for Creatinine/Specific Gravity/pH.
In the rare case where there is an invalid UDT (as indicated by the “invalid” bar on the IA), repeat the test immediately (on the same sample first in case it was simply a defective IA dip). Similarly, if one of the tampering indicators was abnormal, ask the patient to urinate again if possible and repeat the test.
Patient Debrief
Show the patient the IA results, and enter them into START-IT along with the indicators for tampering as applicable. With the click of a button the report is deposited into the patient’s chart in the EMR (assuming OCEAN platform is being used, and you have one of the compatible EMRs). If there is an unexpected result, the patient may have an explanation which you can pass along to the physician. For other aspects of handling “unexpected” results, see Appendix II.
Patient Fails to Attend
Also of note, if a patient is booked for a UDT but does not attend the appointment (no-show, cancellation), then the patient should be added to the recall list in the Randomization Spreadsheet (your masterlist document – Chapters 2-4). Similarly, if the patient says that he/she is unable to urinate, you can either add them to the recall list, or if the schedule permits, keep the patient in the clinic drinking water and simply obtain the sample later in the clinic. For how to respond to repeated failures to attend, see Appendix II.
Cases

Case 1
You wonder about whether you should do LC-MS and/or IA, at the office or at the lab?
There are several considerations here including human resources, patient distance from the clinic/lab, and pros and cons of both tests. Clinical policy decisions such as this are discussed further in Appendix I.
Case 2
The patient has provided a urine sample and you are analyzing it. BZD has a very faint 2nd line. Is this positive or negative?
This scenario comes up repeatedly - as long as you can see that 2nd line, the result for that panel is negative (even if very faint).
Case 3
Are taping and temperature taking really necessary?
We have been doing this for greater than 5 years now and have only had one temperature that was too cold, and no abnormal results for creatinine, specific gravity or pH. You may consider not using these given their apparently low-yield. See Appendix III: Anti-tampering Techniques.
Case 4
Our clinic is unable to use START-IT - how should we collect and conduct IA in the clinic?
This is challenging but possible. Prior to creating START-IT, we used paper self-reports which also had a section where the staff conducting the test could write IA results. We then had this paper scanned to the chart and interpreted by the physician. We have START-IT available online that does not require the OCEAN platform, in which case you can do START-IT in a web browser and then copy and paste the interpretation into any EMR chart.
Chapter Pearls

- Organized collection of not just the UDT itself, but prescribed and non-prescribed medications, are important to ensuring an accurate interpretation.
- UDT can be conducted in a discreet and humane manner.
- Be careful if the patient asks what a result means - if you are not trained in UDT interpretation then it may be worth leaving to the physician. There are false positives (ex. morphine panel is positive even when he/she didn’t actually take morphine), and false negatives (ex. oxycodone panel is negative even when he/she took oxycodone recently).
- A urine sample must be labelled correctly. In the case of LC-MS, as accurate as it is, if the label is for the wrong patient then you will have erroneous interpretations and potentially disastrous management changes. Preventing results from going under the wrong patient is one reason it is helpful to both input the initials into START-IT (to prevent human error of uploading to the wrong patient chart), and to show the result to the patient so that there are no surprises and he/she can accept or deny the result implication on-the-spot.
- If technical questions arise, feel free to contact our Addictions and Pain Care Coordinator at
 . This staff member has a wealth of knowledge about the technical process of conducting UDT in the office and has been doing it at our clinic for years.
. This staff member has a wealth of knowledge about the technical process of conducting UDT in the office and has been doing it at our clinic for years.
Now that UDT has been collected and analyzed, let’s look more closely at the START-IT tool for automated IA interpretation…
