Now that a list of patients has been generated to provide a UDT, let’s go over the booking procedures…
Your clinic will have to decide on whether it would like to do point-of-care testing (IA), and/or confirmatory testing (LC-MS), as well as how appointments will be structured at the clinic. See Appendix I for considerations when making these decisions. At our clinic we use both methods of UDT, and hold two UDT clinics per week (½ day each).
The following assumes your clinic has the capacity and desire to do IA urine drug testing. If it does not, the same protocols can apply except instead of providing a UDT at the clinic, the patient can either provide one for LC-MS directly at the lab, or at the clinic which in-turn sends the sample to the lab for LC-MS analysis.
At this point, the UDT selection process (Chapter 3) has generated a booking list for the month, and these patients will be booked at some point in the coming month. There will also likely be a list of patients on the “Recall list” from previous months that have not provided UDT despite being selected. If your clinic holds 8 UDT clinics per month, then patients on these lists could be divided roughly equally between the clinics. The patient is phoned the morning before the planned appointment. Ideally, UDT will be provided within 36 hours (i.e. same day or next).
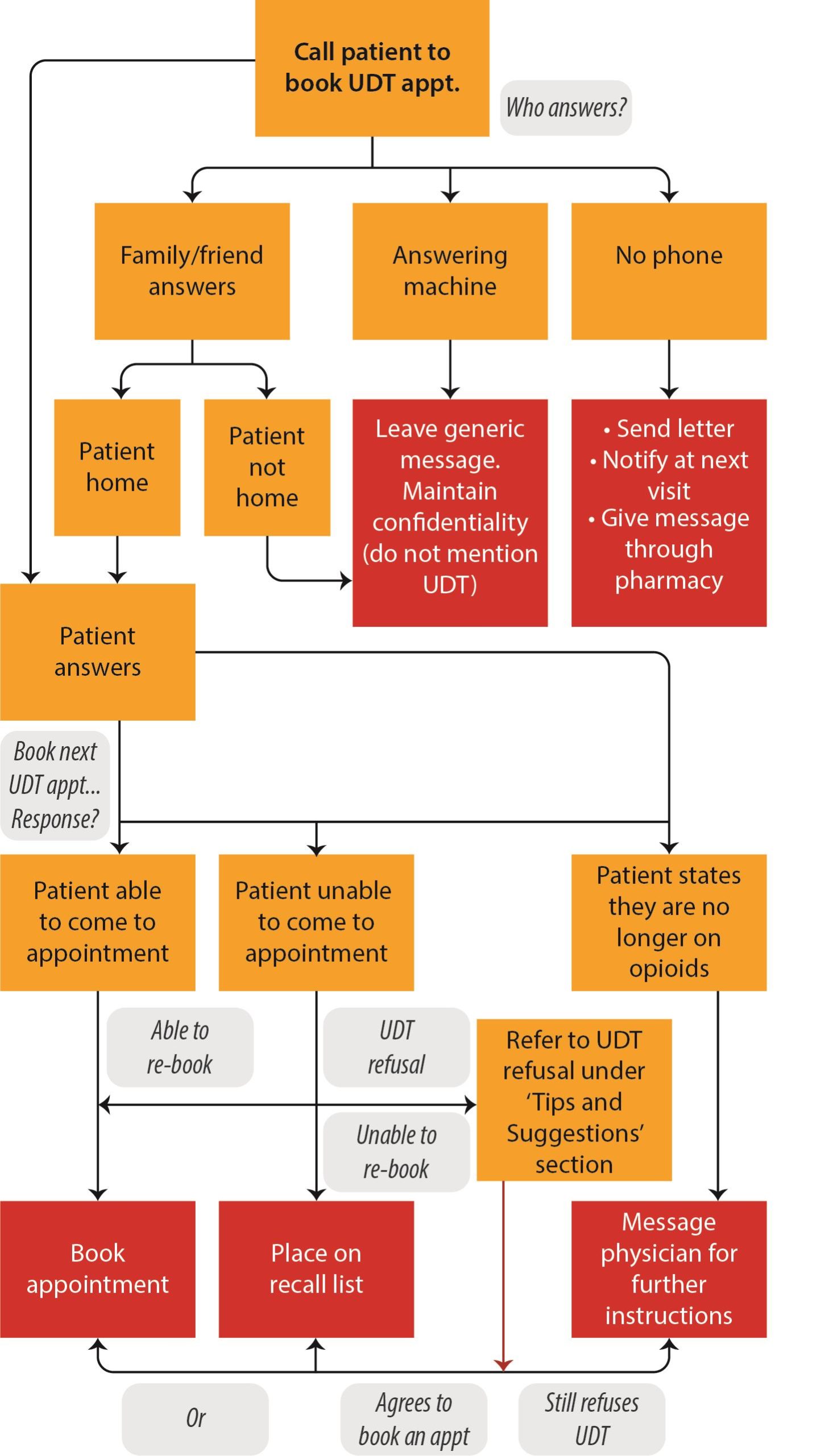
For suggestions on how to handle the various situations that may arise when phoning patients see the schematic below.
While not depicted explicitly here, if you are unable to even reach the patient after numerous attempts (answering machine, no phone, etc) then you will place the patient on the recall list so that he/she will not “fall through the cracks”. You will also message the physician for further instructions. While we don’t provide a “hard and fast” number, if you have tried at least 3 times over 2 weeks and been unsuccessful at reaching the patient or hearing back from them, then consider adding them to the recall list and messaging the physician.
Cases

Case 1
You are the administrator for the HARMS Program at your clinic and Mr. Smith is randomized to be selected for this month. You call the number on file and the patient answers. You tell him you have an appointment for him tomorrow to provide a UDT. He says he doesn’t have to do UDT, and that his physician never spoke to him about it. How do you respond?
This scenario was rare at our clinic, as all patients in the program had already had a discussion and signed a treatment agreement and consent. If your clinic was unable to do this however, then it is still worthwhile to follow the schematic, which in this case will likely lead to messaging the physician for further instructions. Physician may then discuss the program with the patient to initiate the process for consenting +/- completion of treatment agreement.
Case 2
You are the administrator for the HARMS Program at your clinic and Mr. Johnston is randomized to be selected for this month. You leave a message on the voicemail to call the clinic back. He doesn’t call back, so you call him again the following week and leave another message. He still doesn’t call back. What do you do at this point?
Consider trying one more time, or trying an alternate phone number, and if still no response then add him to the recall list (will try again next month) and consider notifying the physician.
Tips and Suggestions
Start of conversation: “You’ve been randomly selected through our opioid safety program to provide a urine drug test. This program applies to all patients at our clinic prescribed opioids for chronic pain. We will try and book you within the next 1-2 days, are you able to attend an appointment tomorrow?”
Patient asks why he/she has to do UDT, say: “Our clinic is using urine drug testing for everyone at the clinic prescribed opioids for chronic pain. It is a safety measure given the potential harms of these medications. Testing selection is random, and typically infrequent. ”
Patient refuses UDT: “You’re aware that this is an expectation of patients at our clinic prescribed opioids for chronic pain? I will notify your physician – is there a particular reason you would like me to tell him/her about why you are declining to provide a UDT?”
Other Reminders
Patient does not book an appointment (for whatever reason) – make sure to add to recall list of Randomization spreadsheet.
Updating the master list: once patient is booked for an appointment, consider marking this by bolding the name on the UDT Selection tab for that month. That way you will know who still has to be booked. If patient ends up cancelling that appointment (or no-showing) and not re-booking right away, add the patient to the “Recall list” (See Chapter 3).
A note about notification time: while ideally the patient is booked in <36h from the time of notification, this is of course not always possible (work commitments, etc). If patient is unable to make this, then book for next time when patient is available. If not available to come to clinic within the next several weeks, at the discretion of your own clinic HARMS policy (See Appendix I: Choosing a method for UDT), you may offer to the patient to provide a UDT at the lab (they tend to be open more hours than UDT clinics). Patient can either pick up requisition at the clinic, or as applicable have req sent directly to their lab.
Chapter Pearls

- UDT has the potential for significant inconvenience for patients (hence why for low risk patients where safety is less of a concern, it is conducted infrequently). The 36 hour from notification to provision of a sample is a goal, but is not possible in everyone. In these cases, book when it’s convenient for the patient.
- The Recall list is an important way to keep track of people that are randomized but not providing UDT. In our original experience, patients like this would often fall through the cracks. Perhaps ironically, but not surprisingly, the patients that are consistently busy, cancelling and no-showing are the ones who are often eventually identified as being “harmed”.
Now that patient is booked for a UDT, let’s cover how the UDT may be conducted at the clinic…
