While diagnosing Opioid Use Disorder and getting the patient on-board with new treatment strategies can be one of the most challenging tasks with opioids in CNCP, it is important to familiarize yourself with the steps following diagnosis…
Opioid use disorder (OUD) is the DSM-V diagnosis for opioid addiction. There are numerous technical elements that we could cover (specific criteria including whether OUD is mild/moderate/severe, previous terminology that is still used like Opioid Dependence and Opioid Abuse, etc.), however instead of “reinventing the wheel”, this section will simply cite other references for the more technical components of OUD. The material here will focus on some of the practical elements of how to help these patients suffering with addiction. Specifically, it addresses those patients originally seen for “chronic pain” who are subsequently identified as having challenges with addiction.
The diagnosis:
It is very helpful to remember here that “pain” and “addiction” are not mutually exclusive, black-and-white terms. It is best thought of as a spectrum. With patients on the addiction side, in an ideal world the patient is willing to acknowledge the problem. This is unfortunately often not the case, so instead we must rely on other means of assessing the patient. The main pattern with addiction is one of escalating use and increasing dysfunction, leading to further escalating use and further increasing dysfunction. Patients may try to hide this pattern – insisting that the opioids are helping them. By applying universal UDT to all patients with chronic pain prescribed opioids, we may pick up on subtle concerns, gradually tighten control/monitoring, and if addiction is finally established then we can intervene and support the patient accordingly.
Initial discussion:
Support, support, support! We are not here to punish anyone. We have very good biological treatments for opioid addiction and if we can maintain a therapeutic alliance then we can help reduce the patient’s suffering. See Appendix VI.
Overall approach:
While the majority of opioid use disorder in Canada is treated in high-volume specialty clinics, research suggests that better care is provided under the auspices of family physicians1. This is one reason that, if you have the time and energy to learn, it can be immensely beneficial to your patient – and rewarding to yourself – to offer Opioid Agonist Treatment (OAT) for opioid use disorder. While beyond the scope of this manual, we are working on doing for Opioid Use Disorder what we have done for UDT in chronic pain. We have simple innovations that address existing barriers and can help bring OAT into frontline family medicine. There are numerous educational resources available online – and new ones coming out regularly – but we think it’s important to address the barriers to uptake at the level of frontline clinicians. This requires practical tools: simple, versatile and effective. Stay tuned for more about this initiative.
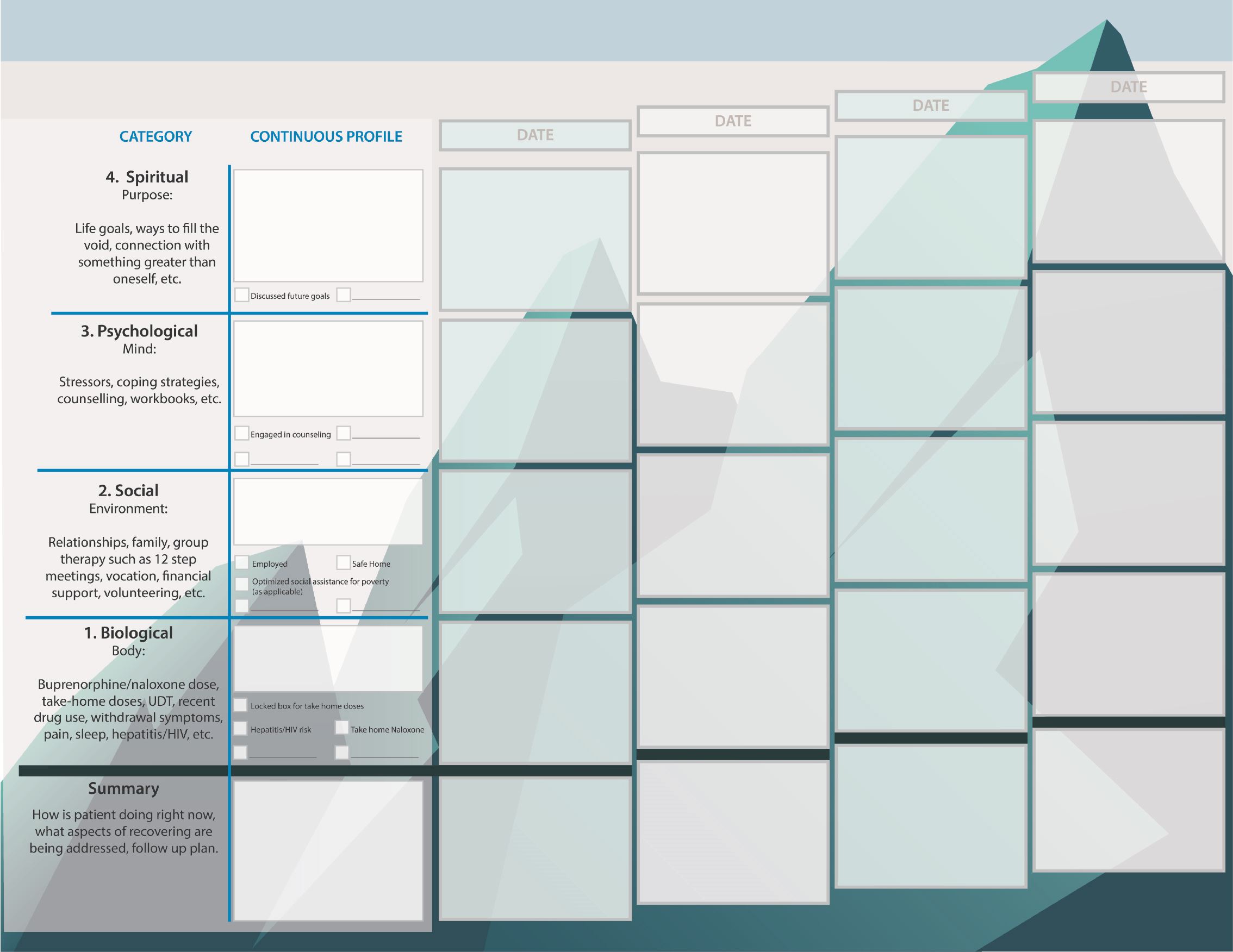
For the purposes of this manual, suffice it to say that every approach to addictions treatment involves reducing stress/pain/suffering, and/or improving coping/resilience. These strategies occur across the domains of biopsychosocial-spiritual (body, mind, environment and sense of purpose). Typically, earliest interventions address the biological aspects of recovery (eg. withdrawal) since it tends to be difficult to advance to deeper levels of recovery without first addressing these more superficial ones. The flowsheet infographic below demonstrates this approach as being analogous to climbing a mountain – with biological challenges being the first to ascend, followed by social, psychological and finally spiritual. This infographic is part of an addictions flowsheet that we have been using in clinical practice for over 5 years. It can be immensely valuable when a patient in the throes of addiction presents to clinic and his/her life seems so disastrous that you don’t know where to begin. It also organizes notes easily. We are currently applying for grants to upgrade and improve the rest of our addictions flowsheet (not pictured here).
Buprenorphine/Naloxone Visit Flowsheet
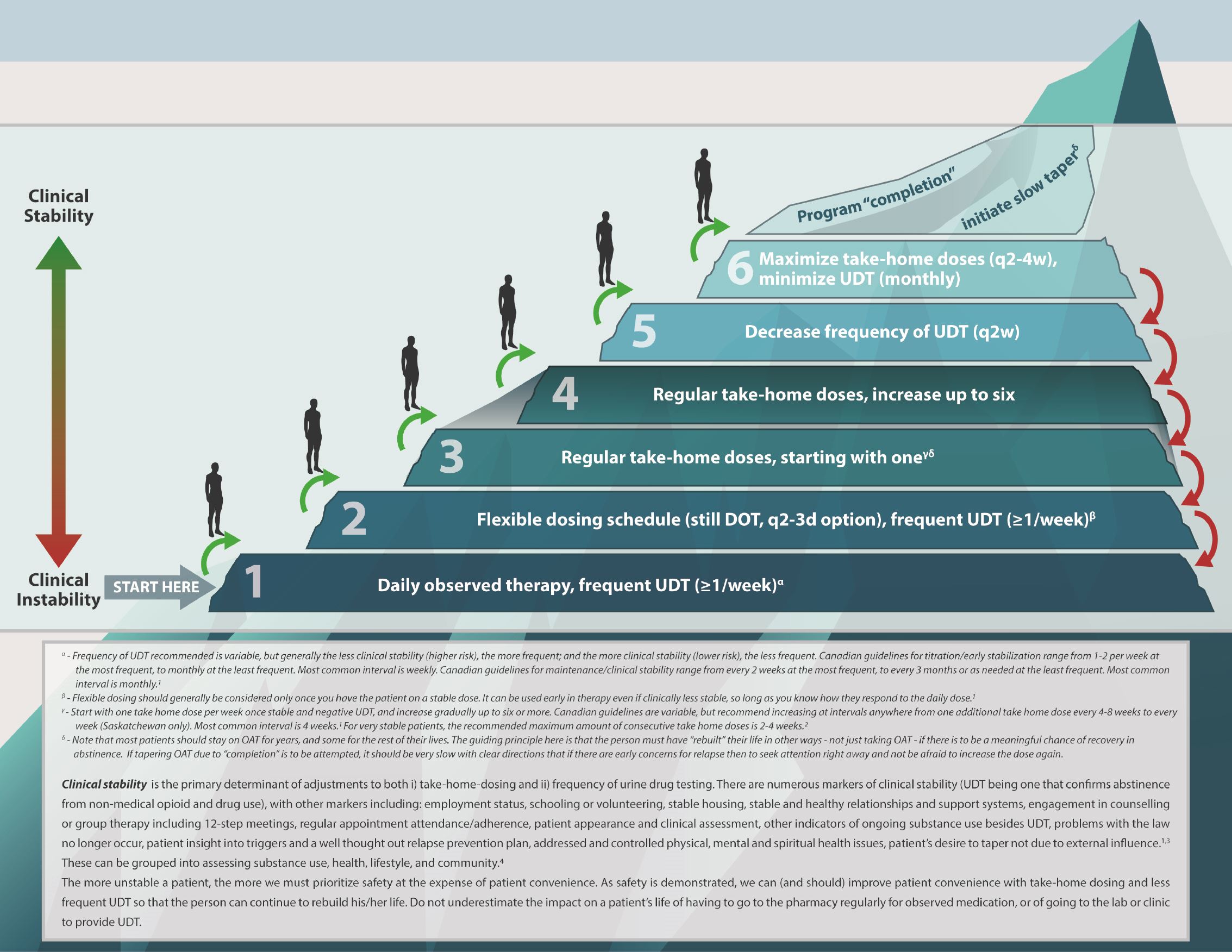
The following infographic provides a common-sense visual for how we address take-home doses and UDT frequency when prescribing OAT. Essentially, clinical stability is the primary determinant, and UDT is simply one indicator of that clinical stability (others include stable relationships and housing, work, engagement in counselling, etc.). A more stable patient has more take-home doses and less UDT, and a less stable patient has less take-home doses and more UDT. In the unstable patient, less take-home-doses and more frequent UDT are in the interest of safety and come at the expense of patient convenience. Conversely, if someone demonstrates improving clinical stability (through UDT results and other markers), then in the interest of patient convenience and supporting one’s recovery, decreasing the burdensome pharmacy visits and UDT is generally indicated.
Buprenorphine/naloxone Prescribing and Monitoring Ladder
There are numerous resources out there that can help with the educational challenges around prescribing buprenorphine/naloxone agonist treatment. We have found the following particularly useful:
- Bruneau J, Ahamad K, Goyer M-È, et al. Management of opioid use disorders: a national clinical practice guideline. CMAJ. 2018;190(9):E247-E257. doi:10.1503/cmaj.170958
- Kahan M, Hardy K, Clarke S. Safe opioid prescribing and managing opioid use disorder: A pocket reference for primary care providers. December 2017. https://www.womenscollegehospital.ca/assets/pdf/MetaPhi/2017-12-19%20PCP%20safe%20opioid%20prescribing.pdf.
- Kahan M, Srivastava A, Ordean A, Cirone S. Buprenorphine: New treatment of opioid addiction in primary care. Canadian Family Physician. 2011;57(3):281-289.
- Ducharme S, Fraser R, Gill K. Update on the clinical use of buprenorphine: in opioid-related disorders. Can Fam Physician. 2012;58(1):37-41.
- Handford C, Kahan M, Srivastava A, et al. Buprenorphine/Naloxone for Opioid Dependence: Clinical Practice Guidelines. 2011. http://cpsa.ca/wp-content/uploads/2015/07/buprenorphine_ naloxone_CAMH2012.pdf.
- MacMaster University Health Sciences. (2017) Opioids Clinical Primer. https://machealth.ca/programs/opioids_clinical_primer/
Note again that our next project (after HARMS) is to translate knowledge into practice with Opioid Use Disorder. We aim to increase uptake of buprenorphine/naloxone agonist treatment in primary care through formalizing and disseminating the innovative tools we have been using in our clinical practice for several years. While family physicians are being inundated with resources for more education around OUD and OAT, there is still a paucity of pragmatic clinical tools that help frontline physicians at the level of knowledge translation.
Cases

Case 1
A 40 year old male, who has been a patient of yours for many years, has requested early refills of his prescription several times in the last year. He has fibromyalgia, and you are currently prescribing oxycodone/acetaminophen 8 tabs/day. His wife came in for an appointment and tells you that her husband is buying medications from the street, his health is declining, he is depressed and generally unwell. When you discuss with him at his next appointment, he states he has to buy from the street because the oxycodone no longer controls his pain. What do you do?
This patient, by clinical Gestalt, appears to have OUD given that his use has been escalating as his function has been declining. Ideally you can get him on board to start treatment. See previous chapters for discussion points. In terms of actual treatment, this patient would be an excellent candidate for OAT with buprenorphine/naloxone. If he denies that he has OUD, then at your discretion you may consider prescribing buprenorphine/naloxone for pain (off-label - BID to QID) which has the added benefits over his existing oxycodone prescription of lower overdose potential, and tighter affinity for the opioid receptors (such that ongoing oxycodone use would not be rewarding to the patient). The induction of buprenorphine/naloxine is beyond the scope of this manual.
Case 2
A 52 year old male has been a patient of yours for about 5 years. After a diagnosis of OUD 9 months ago, you started him on OAT right away with buprenorphine/naloxone. He was successfully titrated to a sublingual dose of 12 mg once daily Although he has complete relief of withdrawal symptoms and cravings, functions well, and is deemed clinically stable, you have noticed a sharp decline in his mood at the past two visits. After doing some probing, the patient opens up to you that even though he has improved his life, his opioid problem has caused a break down in the relationship with his kids. He states that “I physically feel good, but I feel as though I have no one outside of the clinic to talk to about my problems, and as a result, am feeling more and more anxious.” How do you approach this situation?
This is an example demonstrating that OAT is only one aspect of treatment. Although he is doing well with the physical aspect of his recovery (withdrawal is controlled), there are other aspects of his life that may need to be addressed. There are other aspects of pain/suffering, in addition to the physical ones, that need to be addressed if patient is to maximize his chance of a successful long-term recovery. With the patient opening up, this is a great opportunity to advance in addressing the other aspects of recovery (such as seeing a counsellor). Beyond the scope of this manual, however considerations include the relationship with his kids, work, past-trauma, etc. A helpful forum to address these various issues may be 12-step meetings, addictions counselling, rehabilitation programs, etc.
Case 3
A 23 year old female has been treated for OUD with buprenorphine/naloxone at your clinic for about 6 weeks now. She is doing better and is maintained on a dose of 16 mg daily, however, her LC-MS UDT 2 weeks ago was positive for methamphetamine and clonazepam that is not prescribed. She discloses to you that she met up with an old friend two weeks ago and had taken the two drugs at a party. All other UDT’s have come back negative. She comes in for a follow up appointment this week and asks about take home doses and why she has to provide a UDT every week.
This is a great opportunity to speak with the patient about take home doses and frequency of UDT. Remember that UDT is one marker of clinical stability. If this patient had an unexpected UDT, but was working again, in a new stable relationship, etc. then perhaps take-home dose(s) would be justified. Use your clinical discretion but remember that UDT is just one marker of clinical stability when considering how many take-home doses to give, and how often to conduct UDT. You can tell her that the frequency of UDT decreases as she demonstrates that she is doing well (“clinically stable”).
Chapter Pearls

- OUD is best treated in primary care. OAT with buprenorphine/naloxone is the first-line treatment for almost all patients with OUD.
- OAT is only one aspect of treatment for OUD. To have the best chance of long-term success, other aspects of recovery need to be addressed as well.
- Clinical stability is the main determinant of take-home doses and UDT frequency when prescribing OAT (very similar to the general idea in the HARMS Program for patients with CNCP, as demonstrated in the Risk Ladder). UDT is one marker of clinical stability.
- Harm reduction should be employed by providing naloxone kits to all patients prescribed OAT.
REFERENCES:
- Perry D, Orrantia E, Garrison S. Treating opioid use disorder in primary care. Can Fam Physician Med Fam Can. 2019;65(2):117.
